Table of Contents
- Introduction
- What Does “Kill Tooth Pain Nerve in 3 Seconds Permanently” Really Mean?
- Benefits & Advantages of Permanent Nerve Treatment
- How Professional Endodontic Treatment Works: A Step-by-Step Process
- Comparison With Common Alternatives
- Cost Breakdown & Pricing Factors for Permanent Solutions
- Aftercare & Long-Term Maintenance
- Common Problems & Real Solutions
- Signs Your Tooth Nerve Is Damaged
- Expert Insights & Real-World Examples
- FAQs About Tooth Nerve Treatment
- Conclusion & Next Steps
- Summary & Key Takeaways
1️⃣ Introduction
Severe, throbbing tooth pain can feel like an emergency that demands immediate, permanent relief. If you’ve searched for ways to kill tooth pain nerve in 3 seconds permanently, you’re likely experiencing that desperate, urgent discomfort that makes concentration impossible and life unbearable. This intense pain typically originates from the dental pulp—the innermost part of your tooth containing nerves, blood vessels, and connective tissue. When this pulp becomes infected or inflamed due to deep decay, trauma, or cracks, the resulting pain can be excruciating. While the idea of instantly and permanently eliminating this nerve pain is compelling, understanding the reality of dental treatment is crucial for making informed, safe decisions about your oral health. This comprehensive guide will explore what permanent nerve treatment actually entails, separate myth from medical reality, and provide you with the expert knowledge needed to address severe tooth pain effectively and safely for long-term health.
The search for immediate, permanent solutions reflects genuine suffering and a desire for definitive resolution. However, responsible dental care requires precision, proper diagnosis, and sterile technique to not only address pain but also preserve tooth structure and prevent future complications. This article will delve deep into the professional procedures that come closest to achieving what the phrase kill tooth pain nerve in 3 seconds permanently suggests, while maintaining the highest standards of safety, efficacy, and long-term oral health. We’ll examine why certain promises are unrealistic, what truly effective treatments involve, and how you can achieve lasting relief through evidence-based dental science.
2️⃣ What is “Kill Tooth Pain Nerve in 3 Seconds Permanently”?
The phrase kill tooth pain nerve in 3 seconds permanently is a search query that represents a patient’s ultimate desire: immediate, complete, and everlasting relief from debilitating toothache. In dental terminology, this concept most closely aligns with pulpectomy—the complete removal of the diseased dental pulp from the crown and roots of a tooth—or its more commonly known form, root canal therapy. However, the “3 seconds” aspect is a significant oversimplification of a meticulous medical procedure that requires precision, anesthesia, and sterile technique to ensure both effectiveness and safety.
From a biological perspective, the “nerve” in question is part of the dental pulp, a complex tissue containing nerves (which transmit pain), blood vessels (which provide nutrients), and connective tissue. When this pulp becomes irreversibly inflamed or necrotic (dead) due to bacterial infection from deep cavities, fractures, or trauma, the pain signals can be intense. “Killing” this nerve tissue permanently means completely removing or devitalizing this pulp tissue in a way that prevents any future sensation or infection in that chamber. In professional dentistry, this is achieved through endodontic therapy, which involves accessing the pulp chamber, removing all pulpal tissue, disinfecting the intricate root canal system, and sealing it with inert material to prevent re-infection.
It’s crucial to understand that the pain relief during treatment isn’t instantaneous in the literal three-second sense. While the local anesthetic injection itself can numb sensation within minutes, the actual permanent elimination of the nerve tissue is a process that takes place over the course of the procedure. The profound relief comes once the source of inflammation—the pressurized, infected pulp—is removed. The “permanent” aspect is accurate when the procedure is completed correctly: once the pulp is removed, it doesn’t regenerate. The tooth becomes non-vital but can remain fully functional for decades with proper restoration and care. This distinguishes true endodontic treatment from temporary painkillers or home remedies that merely mask symptoms without addressing the underlying pathological cause.
The reality is that no safe, effective dental procedure can be completed in three seconds. Even the administration of local anesthesia takes longer than three seconds to perform properly. What patients perceive as the “killing” of the nerve—the moment when the pain stops—typically occurs once the dentist accesses the pulp chamber and relieves the pressure from the inflamed tissue. This can bring dramatic relief, but the complete, permanent treatment requires additional time for cleaning, shaping, and sealing the canals to prevent future problems. Understanding this distinction is key to setting realistic expectations and avoiding dangerous attempts at self-treatment or seeking unqualified providers who promise impossible results.
3️⃣ Benefits & Advantages of Permanent Nerve Treatment

Choosing professional, permanent nerve treatment through root canal therapy offers substantial advantages over temporary pain management or tooth extraction. The most immediate and profound benefit is the complete elimination of the acute pain caused by the inflamed or infected pulp. Once the diseased tissue is removed, the toothache that may have been constant, throbbing, and severe disappears. This relief isn’t merely masked with analgesics; it’s resolved at its source. The tooth itself becomes asymptomatic, allowing patients to eat, sleep, and function without discomfort. This represents a significant improvement in quality of life and daily functioning.
Beyond immediate pain relief, tooth preservation stands as a paramount advantage. The alternative to root canal treatment is typically extraction—complete removal of the tooth. Saving your natural tooth through endodontic therapy maintains your natural bite alignment, prevents neighboring teeth from shifting, and preserves normal chewing function. Natural teeth are more efficient for chewing than even the best artificial replacements. They also provide natural proprioception—the sense of how much force to apply when biting—which helps protect the tooth and supporting structures from excessive force. By choosing to save the tooth, you maintain the integrity of your dental arch and avoid the bone loss that commonly follows extractions.
Another significant advantage is the prevention of infection spread. An infected tooth pulp acts as a reservoir for bacteria that can spread beyond the tooth’s roots into the surrounding bone, creating a dental abscess. This can lead to serious, potentially life-threatening infections that spread to other areas of the head, neck, or even systemically through the bloodstream. By completely removing the infected tissue and sealing the canals, root canal therapy eliminates this source of infection, protecting both your oral and overall health. The procedure effectively contains what could become a more significant health threat.
From a long-term economic perspective, cost-effectiveness makes permanent nerve treatment advantageous. While the initial investment in a root canal and subsequent crown may seem substantial, it’s generally more economical over a lifetime than the alternatives. Tooth replacement options like dental implants or bridges are typically more expensive and involve more extensive procedures on adjacent teeth or bone. Additionally, preserving your natural tooth avoids the ongoing maintenance and potential future replacements associated with prosthetic devices. The treated tooth, when properly restored with a crown, can last a lifetime, making it a wise long-term investment in your oral health.
Aesthetic and functional continuity provides another benefit. Your natural tooth maintains the appearance of your smile without gaps. Even with today’s advanced implants, matching a natural tooth’s exact color, texture, and light transmission can be challenging. Keeping your tooth means no adjustment period for speaking or eating, as sometimes occurs with removable prosthetics. The treated tooth continues to stimulate the surrounding bone through normal function, preventing the ridge resorption that occurs after extraction and can alter facial contours over time. This preservation of natural structure supports both function and appearance throughout your life.
4️⃣ How Professional Endodontic Treatment Works: A Step-by-Step Process

Professional endodontic treatment, the medical reality behind the desire to kill tooth pain nerve in 3 seconds permanently, is a precise, multi-step procedure performed under strict sterile conditions. The process begins with comprehensive diagnosis and imaging. Your dentist or endodontist will examine the tooth, perform vitality tests (like thermal or electric pulp testing), and take diagnostic X-rays, often including a periapical radiograph that shows the entire tooth and surrounding bone. These images reveal the number and shape of root canals, the extent of decay or infection, and any signs of bone loss at the root tips. This diagnostic phase is critical, as missed canals are a common cause of treatment failure.
Once diagnosis confirms the need for treatment, the local anesthesia phase begins. Contrary to myths about root canals being painful, modern anesthesia makes the procedure no more uncomfortable than a routine filling. The dentist administers a local anesthetic like lidocaine or articaine to completely numb the tooth, surrounding gum, and bone. For severely infected teeth where inflammation can neutralize anesthetic, dentists may use supplemental techniques like intraligamentary injections or even conscious sedation for anxious patients. Effective anesthesia ensures a pain-free experience during the procedure, though patients may feel pressure or vibration—not pain.
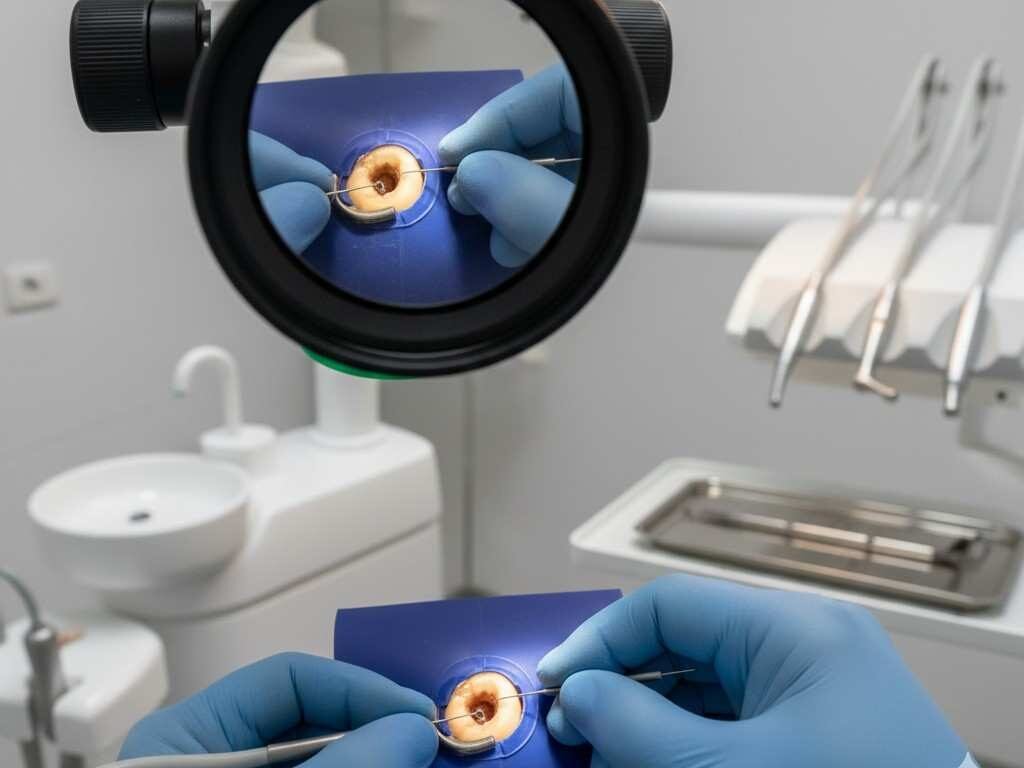
The next phase is isolation and access preparation. The dentist places a rubber dam—a protective sheet—around the tooth to isolate it from the rest of the mouth. This critical step prevents saliva (containing bacteria) from contaminating the root canal system during treatment and protects the patient from accidentally inhaling or swallowing small instruments. Using specialized dental drills, the dentist then creates a small access opening in the crown of the tooth to reach the pulp chamber. This access must be precise to locate all canal openings while preserving as much healthy tooth structure as possible.
The core of the procedure is pulpal tissue removal and canal shaping. Using a series of increasingly fine instruments called endodontic files, the dentist carefully removes the inflamed or necrotic pulp tissue from the pulp chamber and each root canal. The canals are then cleaned, enlarged, and shaped to facilitate thorough disinfection and subsequent filling. During this process, the dentist repeatedly irrigates the canals with antimicrobial solutions like sodium hypochlorite (bleach solution at safe concentrations) to dissolve any remaining tissue and kill bacteria. This mechanical and chemical cleaning is what permanently removes the nerve tissue and addresses the infection—the closest professional equivalent to “killing the nerve.”
After shaping and cleaning, the canals must be completely dried before the obturation phase—filling and sealing the empty canal spaces. The dentist uses an inert, biocompatible material called gutta-percha, a rubber-like substance, in combination with a sealant cement to fill the canal space three-dimensionally. This sealing prevents future bacterial recontamination. The access opening in the crown is then sealed with a temporary or permanent filling. Finally, because the tooth becomes more brittle without its internal pulp, a dental crown is almost always recommended to protect the tooth from fracture under normal chewing forces. This restoration typically occurs in a separate appointment after the endodontic treatment has healed.
5️⃣ Comparison With Alternatives
When facing severe tooth pain from nerve inflammation, patients have several options beyond professional endodontic treatment. Understanding the differences in effectiveness, longevity, cost, and impact on oral health is crucial for making an informed decision. Below is a detailed comparison of permanent nerve treatment (root canal therapy) against the most common alternatives.
Detailed Comparison Table: Permanent Nerve Treatment vs. Alternatives
| Treatment Aspect | Root Canal Therapy + Crown | Tooth Extraction Only | Temporary Pain Management | Dental Implant After Extraction |
|---|---|---|---|---|
| Pain Resolution | Permanent elimination of source pain; tooth becomes asymptomatic | Immediate relief from toothache, but surgical site pain during healing | Temporary masking of symptoms; pain returns when medication wears off | No tooth pain after healing, but surgical discomfort from implant placement |
| Procedure Time | 1-3 appointments (90-120 minutes each) | Single appointment (20-40 minutes) | Immediate (minutes for medication) | Multiple appointments over 3-9 months |
| Longevity | 85-95% success rate at 10+ years; can last lifetime with proper care | Permanent tooth loss; space remains unless replaced | Hours to days of relief only | 95%+ success at 10 years; can last 25+ years with maintenance |
| Cost (Estimated) | $1,000-$2,500 (depending on tooth and geographic location) | $150-$450 for simple extraction | $10-$50 for OTC/prescription pain relievers | $3,000-$6,000+ per implant with crown |
| Oral Health Impact | Preserves natural tooth, bone, and arch integrity; maintains chewing function | Bone resorption over time; adjacent teeth may shift; chewing efficiency reduced | No treatment of underlying cause; infection can spread | Prevents bone loss at site; preserves chewing but requires adjacent teeth remain untouched |
| Aesthetic Outcome | Natural tooth preserved; crown matches adjacent teeth | Visible gap unless replaced; potential facial collapse over time | No change in appearance | Natural-looking replacement but may not match adjacent teeth perfectly |
| Risk Factors | Possible procedural complications (missed canals, instrument separation); requires crown to prevent fracture | Surgical risks (dry socket, nerve injury); long-term consequences of tooth loss | Medication side effects; risk of overdose; infection progression | Surgical risks; possibility of implant failure or peri-implantitis |
| Recovery Time | Minimal; mild discomfort for few days; normal function after crown placement | 1-2 weeks for soft tissue healing; months for bone remodeling | Immediate but temporary | 3-6 months for osseointegration before final crown |
| Insurance Coverage | Typically 50-80% coverage for endodontics; 50% for crown (subject to plan limits) | Usually 70-80% coverage for extractions | Varies; OTC medications not typically covered | Often limited coverage; may be considered elective |
Tooth extraction may seem like a simpler, more immediate solution, but it introduces long-term consequences. While extraction removes the painful tooth, it creates a vacancy that leads to dental drift (neighboring teeth shifting into the space), opposing tooth supra-eruption (the opposing tooth growing longer without contact), and alveolar bone resorption (the jawbone shrinking where the tooth root is missing). These changes can affect bite alignment, chewing efficiency, and facial aesthetics over years. Extraction might cost less immediately but often leads to higher long-term expenses when considering replacement options or orthodontic correction of shifted teeth.
Temporary pain management through over-the-counter or prescription medications provides only symptomatic relief. NSAIDs like ibuprofen can reduce inflammation and pain, while analgesics like acetaminophen address pain only. Antibiotics may temporarily control infection but cannot reach the necrotic tissue inside the root canals effectively. This approach risks allowing the infection to spread, potentially leading to cellulitis (soft tissue infection), abscess formation, or systemic infection. It addresses neither the source of pain nor the underlying pathology, serving only as a stopgap until definitive treatment can be obtained.
Dental implants represent a high-quality replacement option after extraction but are not a direct alternative to saving the natural tooth. The implant process is more invasive, time-consuming, and costly than root canal therapy. It involves surgical placement of a titanium post into the jawbone, followed by a months-long healing period for osseointegration (bone fusing to the implant), before finally placing a crown. While implants have excellent success rates, they lack the periodontal ligament that provides cushioning and sensory feedback during chewing. The ADA Council on Scientific Affairs notes that preserving the natural tooth through root canal treatment, when possible, is generally the preferred first option due to its predictability and preservation of natural structure.
Pulp capping and pulpotomy are more conservative alternatives for less severely inflamed pulp, but they are not applicable when irreversible pulpitis or necrosis has occurred. These procedures attempt to preserve pulp vitality by removing only the affected portion, but they require specific conditions: minimal inflammation, mechanical exposure during cavity preparation, and the pulp’s ability to heal. For the severe pain that prompts searches to kill tooth pain nerve in 3 seconds permanently, these conservative options are typically not viable because the inflammation has progressed beyond the point of reversibility.
6️⃣ Cost Breakdown & Pricing Factors

Understanding the financial investment required for permanent nerve treatment helps patients plan appropriately and avoid being surprised by unexpected expenses. The total cost to kill tooth pain nerve professionally through root canal therapy and subsequent restoration typically ranges from $1,000 to $3,500 per tooth in the United States, with significant variation based on multiple factors. This represents a complete treatment package rather than a single procedure, as addressing the nerve is only part of the solution—the tooth must also be protected from future fracture.
The endodontic treatment itself constitutes a major portion of the cost. Fees vary primarily by tooth type: anterior teeth (front teeth) with single, straight canals typically cost $700-$1,200; premolars with 1-2 canals range from $800-$1,500; and molars with 3-4 or more complex canals cost $1,000-$2,200 or more. This pricing reflects the procedure complexity: molars are harder to access, often have curved or narrow canals that require specialized equipment like dental operating microscopes, and take significantly more time (90-150 minutes versus 45-60 for anterior teeth). Geographic location dramatically affects pricing, with urban coastal areas typically charging 30-50% more than rural or Midwestern practices.
Restoration costs following the root canal are equally important and often overlooked in initial estimates. After the nerve is removed, the tooth becomes more brittle and requires protection. A dental crown (cap) typically costs $1,000-$2,500 depending on material: full-metal (least expensive), porcelain-fused-to-metal ($1,000-$1,500), or all-ceramic/zirconia ($1,200-$2,500). Some teeth, particularly anterior teeth with minimal prior decay, may be restored with a permanent filling instead of a crown ($150-$450), but this is less common for posterior teeth that bear chewing forces. The core build-up—filling material placed inside the tooth to support the crown—adds another $200-$500 if substantial tooth structure is missing.
Diagnostic and ancillary costs include the initial examination ($50-$150), diagnostic X-rays ($25-$200), and possibly cone-beam computed tomography (CBCT) for complex cases ($200-$500). CBCT provides 3D imaging that reveals additional canals, root fractures, or complex anatomy not visible on standard 2D X-rays. Retreatment of a previously failed root canal costs 30-50% more than initial treatment due to the complexity of removing existing filling materials and addressing persistent infection. Apicoectomy (surgical root-end removal) for persistent infection after conventional treatment adds $900-$2,000.
Dental insurance coverage significantly impacts out-of-pocket expenses. Most plans cover 50-80% of endodontic treatment after meeting the deductible, typically with an annual maximum of $1,000-$2,500. Crown coverage is often 50% and may fall under a separate “prosthodontics” category with its own annual maximum. Many insurance plans have a missing tooth clause that denies coverage for crowns on teeth that were already missing before policy inception, so verifying benefits is crucial. Payment plans, dental savings plans (not insurance but discount networks), and financing through companies like CareCredit or LendingClub can help manage costs.
Specialist care involves additional considerations. While general dentists perform approximately 70% of root canals, complex cases may be referred to endodontists (root canal specialists). Endodontists charge 20-50% more than general dentists but bring advanced training, specialized equipment like operating microscopes, and higher reported success rates for complex cases. The decision involves weighing higher immediate cost against potentially better long-term outcomes and reduced risk of complications. For straightforward anterior or premolar cases, a skilled general dentist may provide excellent care at lower cost; for complex molars, retreated teeth, or cases with unusual anatomy, specialist care may be worth the investment.
7️⃣ Aftercare / Maintenance Tips

Proper aftercare following endodontic treatment is essential for ensuring the long-term success of your procedure and achieving the “permanent” relief you sought when searching to kill tooth pain nerve in 3 seconds permanently. Immediately following your appointment, you may experience mild to moderate discomfort for a few days as the localized inflammation from the procedure resolves. This is normal and differs significantly from the intense, throbbing pain of the original infection. Your dentist will likely recommend over-the-counter pain relievers like ibuprofen (Advil) or naproxen (Aleve), which reduce inflammation in addition to providing pain relief. For more significant discomfort, prescription medications may be provided. Applying an ice pack to the outside of your cheek in 15-minute intervals during the first 24 hours can also minimize swelling and discomfort.
Oral hygiene practices require specific attention during the healing period. Continue brushing and flossing normally, but be gentle around the treated tooth, especially if a temporary filling is in place. Avoid chewing directly on the treated tooth until it has been fully restored with a permanent crown or filling, as the tooth structure is weakened and more susceptible to fracture. Your dentist may recommend using an antimicrobial mouthwash like chlorhexidine (if prescribed) or alcohol-free formulations to reduce bacterial load in the oral cavity without causing irritation. If a temporary filling falls out, contact your dentist promptly to have it replaced, as this protects the inner seal from saliva contamination.
The interim period between root canal completion and final crown placement is particularly critical. This period typically lasts 2-4 weeks, allowing time for any residual inflammation to resolve before taking final impressions. During this time, the tooth remains vulnerable to fracture, so dietary modifications are essential. Avoid hard, crunchy, or sticky foods like nuts, hard candies, ice, caramel, and chewing gum on that side of your mouth. Cut food into small pieces and chew on the opposite side when possible. If you notice any sharp edges, discomfort from the temporary filling, or signs of the temporary material wearing down, schedule an adjustment with your dentist.
Long-term maintenance of an endodontically treated tooth differs only slightly from caring for natural teeth but includes important considerations. Once the final crown is placed, you can resume normal chewing function, but remember that while the crown is strong, excessive force from habits like bruxism (teeth grinding) or clenching can still cause damage. If you have these parafunctional habits, discuss a night guard with your dentist to protect your investment. Continue regular dental check-ups every six months, as the tooth remains susceptible to new decay at the crown margins or gumline. X-rays at these visits will monitor the bone around the root tips for any signs of healing or potential problems.
Monitoring for potential issues is part of responsible long-term care. While properly performed root canal therapy has high success rates (85-95% at 10+ years), complications can occur. Contact your dentist if you experience: persistent pain or swelling that worsens instead of improving, a visible pimple-like bump (sinus tract) on the gums near the treated tooth, sensitivity to pressure that persists beyond a few weeks, or if the crown feels loose. These could indicate treatment failure, root fracture, or coronal leakage (bacteria entering through the crown margins). Many dentists offer warranties on their endodontic work, so understand what your provider covers and for how long. With proper aftercare and maintenance, your treated tooth can function effectively for decades, providing the permanent solution you sought for your tooth pain.
8️⃣ Common Problems & Real Solutions

Despite high success rates, endodontic treatment can encounter complications that prevent the desired outcome of permanently eliminating tooth pain. Understanding these potential problems and their solutions empowers patients to make informed decisions and seek timely intervention when needed. One of the most frequent issues is post-treatment discomfort that persists beyond the normal healing period. While some sensitivity to pressure for several weeks is normal as the periodontal ligament heals, sharp, spontaneous pain or swelling indicates potential problems. This may result from instrumentation beyond the root apex during cleaning, causing temporary irritation of the bone, or from missed accessory canals that contain residual inflamed tissue. Solutions include allowing additional healing time with anti-inflammatory medication, or in persistent cases, non-surgical retreatment to address missed anatomy.
Vertical root fractures represent a more serious complication that often leads to tooth loss. These cracks originate in the root and propagate toward the crown, typically occurring in endodontically treated teeth that were not properly restored with a crown or that were subjected to excessive forces. Symptoms include vague pain when chewing and possibly a narrow, deep periodontal pocket detectable by your dentist. Unfortunately, teeth with vertical root fractures generally cannot be saved and require extraction. Prevention through proper restoration with a full-coverage crown and avoidance of excessive forces (like chewing hard objects) is crucial. If detected early, some select cases may be treatable with root amputation in multi-rooted teeth.
Persistent or recurrent infection manifests as continued pain, swelling, or the development of a draining sinus tract (gum boil) months or years after treatment. This occurs when bacteria remain in the complex root canal system or re-enter through coronal leakage (micro-gaps between the tooth and restoration). Diagnosis typically involves clinical examination and a cone-beam CT scan to identify the source. Solutions depend on the cause: if the original treatment missed canals or was inadequately cleaned, non-surgical retreatment involves reopening the tooth, removing the existing filling material, and re-cleaning the canals. If infection persists at the root tip despite retreatment, apical surgery (apicoectomy) may be necessary to remove the infected tip and seal the end of the root.
Coronal leakage occurs when bacteria seep between the tooth and its restoration, eventually reaching the filled root canal system. This is a leading cause of long-term failure and underscores why a well-sealed final restoration is as important as the root canal itself. Symptoms may be subtle until significant re-infection occurs. Prevention involves: placing the final crown promptly (within 4 weeks of root canal completion), ensuring proper margin adaptation of the crown to the tooth, and using core build-up materials that bond effectively to tooth structure. If leakage is detected early, replacing the crown with a properly sealed one may solve the problem before significant re-infection occurs.
Calcified canals present a significant procedural challenge, particularly in older patients or teeth that have experienced trauma. Over time, the pulp chamber and canals can fill with secondary dentin, making them narrow, difficult to locate, or impossible to negotiate with standard instruments. Attempting to treat such teeth carries higher risk of perforation (creating an unintended opening in the root) or instrument separation (files breaking inside the canal). Solutions include: referral to an endodontist with specialized equipment like dental operating microscopes and ultrasonic instruments, careful negotiation with specialized small files, and sometimes accepting partial treatment if some canals remain inaccessible. In extreme cases, when canals cannot be negotiated, the alternative may be extraction, though intentional replantation (removing, treating, and replacing the tooth) remains an option in some specialist practices.
Discoloration of the endodontically treated tooth is a common aesthetic concern, particularly for anterior teeth. The tooth may darken over time due to residual pulpal tissue, filling materials, or the natural absence of vitality. While not painful, this can be cosmetically unsatisfactory. Solutions range from internal bleaching (placing bleaching agents inside the tooth chamber) to placing porcelain veneers or full-coverage crowns. Internal bleaching has high success rates for mild to moderate discoloration but may need occasional repetition. For severe discoloration or when other restorations are needed, ceramic crowns provide predictable aesthetic results while strengthening the tooth.
9 Signs That Your Tooth Nerve Is Damaged
Damage to the nerve of your tooth often sends clear warning signals long before the pain becomes unbearable. You may experience sudden sharp pain while eating, lingering sensitivity to hot or cold drinks, throbbing discomfort, or swelling around the tooth — all signs that the nerve is inflamed or infected. Many people searching for ways to Kill Tooth Pain Nerve in 3 Seconds Permanently do not realize that these symptoms actually indicate the problem has already reached deep inside the tooth. Ignoring these warning signs can intensify the pain, pushing patients to desperately seek solutions like Kill Tooth Pain Nerve in 3 Seconds Permanently, instead of addressing the root cause.
The underlying cause of this pain is usually deep decay, a cracked tooth, or repeated dental work that eventually reaches the nerve. Ignoring early symptoms, such as brief sensitivity, often leads to severe, spontaneous pain that disrupts sleep and daily life, trapping patients in the cycle of searching for instant relief. Relying on unverified methods claiming to Kill Tooth Pain Nerve in 3 Seconds Permanently — such as applying aspirin to the gums or using unproven home remedies — is not only ineffective but can further damage the gums and soft tissues.
Recognizing these symptoms early can save your tooth, reduce suffering, and guide you toward a safe and permanent solution, rather than chasing the temporary relief marketed as Kill Tooth Pain Nerve in 3 Seconds Permanently. A dentist can accurately diagnose the issue and provide effective treatment such as a root canal or, if necessary, proper nerve removal, to permanently eliminate the pain. Remember, the only safe and lasting solution to tooth nerve pain comes from professional dental care — not from false promises to Kill Tooth Pain Nerve in 3 Seconds Permanently.
10 Expert Insights & Real-World Examples
Dental professionals bring years of training and clinical experience to the management of severe tooth pain, offering valuable perspectives beyond what patients find through online searches. Dr. Elena Rodriguez, DDS, MS, an endodontist with 15 years of specialist practice, notes: “When patients come to me searching for ways to kill tooth pain nerve in 3 seconds permanently, I understand their desperation. But what they often don’t realize is that the ‘three-second’ concept misses the complexity of what we’re treating. We’re not just silencing a nerve; we’re removing an entire biological system—blood vessels, connective tissue, and nerve fibers—from a complex, microscopic space. Then we must disinfect that space so thoroughly that bacteria cannot survive there, and seal it so completely that no new bacteria can enter. That meticulous process is what creates the ‘permanent’ result they want.”
Real-world case examples illustrate both typical and complex scenarios. Consider Michael, a 42-year-old accountant who presented with severe, throbbing pain in his lower right first molar, exacerbated by lying down and hot liquids. Diagnostic tests confirmed irreversible pulpitis with early periapical involvement. His treatment involved two visits: first to remove the inflamed pulp and place medication, then to complete the cleaning and filling. Michael experienced immediate relief upon pulp removal—the closest moment to “killing the nerve in seconds.” However, the complete procedure took two 90-minute appointments. Five years later, with a zirconia crown protecting the tooth, he remains pain-free with normal function, demonstrating the long-term success possible with proper treatment.
In contrast, Sophia, a 58-year-old teacher, had a previously treated molar that failed after 12 years, with recurrent abscesses. Her case required non-surgical retreatment followed by apical microsurgery when the infection persisted at a tiny accessory canal not visible on standard X-rays. Dr. Rodriguez used a dental operating microscope to locate and treat this canal. “Sophia’s case illustrates why we can’t promise ‘permanent’ in an absolute sense,” she explains. “Biology is complex. But with modern technology like CBCT and operating microscopes, we can address complexities that would have meant extraction just 20 years ago. Her tooth has now been functional for 8 years since retreatment.”
Technological advances have transformed endodontic outcomes. Cone-beam computed tomography (CBCT) provides 3D imaging that reveals additional canals, complex anatomies like C-shaped canals, and minute fractures. Nickel-titanium rotary files allow more precise shaping of curved canals with less risk of ledging or transportation. Dental operating microscopes provide up to 25x magnification with coaxial illumination, enabling visualization of microscopic accessory canals. Electronic apex locators determine working length with over 95% accuracy, reducing reliance on multiple X-rays. These technologies collectively improve success rates from approximately 85% to over 95% for initial treatments in specialist hands.
Expert consensus emphasizes timely intervention. The American Association of Endodontists stresses that delaying treatment for irreversible pulpitis leads to worse outcomes. As infection progresses from the pulp into the periapical bone, treatment complexity increases and success rates decrease slightly. The bacteria shift from primarily aerobic to anaerobic species that are more difficult to eradicate. Bone destruction at the root apex becomes more extensive, requiring longer healing times. This underscores why seeking immediate professional care when experiencing severe tooth pain—rather than searching for instant solutions—leads to better, more predictable outcomes with simpler treatment.
Preventive insights from experts also warrant attention. While not all tooth pain is preventable, many cases originate from untreated decay. Dr. James Chen, a prosthodontist who frequently restores endodontically treated teeth, notes: “The best way to avoid needing to ‘kill the nerve’ is early intervention for cavities. Once decay reaches the pulp, the cascade toward root canal begins. Regular check-ups, proper hygiene, and addressing small cavities promptly are the true ‘three-second permanent solutions’—they prevent the problem entirely. For patients who do need endodontic care, the single most important factor for longevity is the quality of the final restoration. No root canal lasts without a well-sealed crown protecting it from fracture and microleakage.”
11 FAQs (Featured Snippet Optimized)
Q: Can you really kill a tooth nerve in 3 seconds permanently?
A: While the dramatic relief from severe tooth pain can feel instantaneous when a dentist accesses and removes an inflamed pulp, no safe, effective dental procedure can be completed in three seconds. The phrase “kill tooth pain nerve in 3 seconds permanently” represents a patient’s desire for immediate, lasting relief rather than a medical reality. Professional endodontic treatment (root canal therapy) does permanently remove the nerve tissue, but it requires a meticulous procedure lasting 60-120 minutes to properly clean, shape, disinfect, and seal the root canal system. This ensures not only pain relief but also prevents future infection. Attempts to achieve this result in seconds through dangerous methods like applying aspirin directly to the tooth or using caustic substances can cause severe chemical burns to gum tissue without addressing the underlying problem.
Q: What happens when you kill a tooth nerve?
A: When the dental pulp (containing nerves, blood vessels, and connective tissue) is removed during root canal treatment, the tooth becomes non-vital or “dead.” This means: 1) The tooth loses sensitivity to temperature and most sensation (though pressure sensitivity may remain in the surrounding ligament); 2) The tooth no longer receives nutrients from blood vessels, making it slightly more brittle over time; 3) The internal chamber is filled with inert material (gutta-percha) to maintain structure; 4) The tooth remains fully functional for chewing when properly restored with a crown. Importantly, killing the nerve addresses the pain caused by inflammation/infection but doesn’t “kill the tooth”—the mineralized structure remains alive through its attachment to the surrounding bone and gums.
Q: Is it dangerous to kill a tooth nerve?
A: When performed by a trained dental professional using proper sterile technique, endodontic treatment to remove a tooth nerve is a safe, routine procedure with minimal risks. However, attempting to “kill the nerve” through unprofessional means is extremely dangerous. Dangerous methods include: applying aspirin directly (causes chemical burns), using essential oils undiluted (tissue irritation), or attempting DIY extraction (infection, bleeding, damage to adjacent teeth). Professional risks are minimal but can include: temporary post-operative discomfort, slight risk of instrument separation (file breaking in canal), or in rare cases, nerve injury if lower molar roots are near the mandibular nerve. These professional risks are far lower than the risks of untreated dental infection, which can spread to vital spaces.
Q: How long does a tooth last after nerve removal?
A: With proper restoration and care, a tooth that has undergone root canal treatment can last a lifetime. Studies show success rates of 85-95% at 10+ years when treatment is performed to modern standards and followed by appropriate crown placement. The key factors determining longevity are: 1) Quality of the initial endodontic treatment (complete cleaning and sealing); 2) Timely placement of a protective crown (usually within 4 weeks) to prevent fracture; 3) Good oral hygiene to prevent new decay at the crown margins; 4) Regular dental check-ups to monitor for potential issues. Some endodontically treated teeth have remained functional for 30+ years and can outlast many other dental restorations when properly maintained.
Q: Why does my tooth still hurt after a root canal?
A: Some discomfort for several days after root canal treatment is normal as the surrounding bone and ligament heal. However, persistent or severe pain may indicate: 1) Normal healing process (up to 2 weeks of mild sensitivity to pressure); 2) High bite (the crowned tooth contacting first, requiring adjustment); 3) Missed canal containing residual nerve tissue; 4) Root fracture (often causes sharp pain when biting); 5) Persistent infection at root tip; 6) Referred pain from adjacent teeth or TMJ. If pain worsens after 3-5 days or is severe, contact your dentist. They may take an X-ray to check healing, adjust your bite, or prescribe antibiotics if infection is present. Approximately 5-10% of cases may require additional treatment.
Q: Can a tooth nerve heal itself without treatment?
A: Once dental pulp has progressed to irreversible pulpitis (the severe, constant pain that prompts searches to kill the nerve), it cannot heal itself. Unlike other tissues, the pulp is encased in hard dentin with limited blood supply and cannot expand when inflamed. The increased pressure from inflammation cuts off blood flow, leading to necrosis (tissue death). Early, reversible pulpitis (brief sensitivity to cold that subsides quickly) may heal if the cause (like a small cavity) is treated promptly. However, once symptoms include spontaneous pain, pain lasting minutes after stimulus removal, or pain that wakes you at night, the inflammation is irreversible, and the pulp will not recover. Delaying treatment at this stage only allows infection to spread.
Q: What’s the difference between killing a nerve and extracting a tooth?
A: Killing the nerve (root canal) preserves your natural tooth structure by removing only the internal pulp while retaining the outer tooth structure. Extraction removes the entire tooth, root and crown. Key differences: Preservation: Root canal saves your natural tooth; extraction removes it permanently. Function: Saved teeth maintain normal chewing efficiency and prevent bone loss; extraction leads to bone resorption and potential shifting of adjacent teeth. Cost: Root canal + crown typically costs less than extraction + implant replacement. Procedure: Both are performed under local anesthesia, but root canal is more technically complex while extraction is quicker. Long-term: Saved teeth can last a lifetime; extractions create a space that often requires replacement (implant, bridge, or partial denture) to prevent complications.
12 Conclusion + Strong CTA
The search to kill tooth pain nerve in 3 seconds permanently comes from a place of genuine suffering and a desire for definitive relief. As we’ve explored throughout this comprehensive guide, while the literal interpretation of that phrase doesn’t align with dental reality, the underlying desire for immediate, lasting resolution is absolutely achievable through modern endodontic treatment. Root canal therapy represents the professional, evidence-based approach to permanently addressing the source of severe tooth pain by removing diseased pulp tissue, disinfecting the intricate canal system, and sealing it against future infection. This treatment, while requiring more than three seconds, provides the permanent solution that allows you to preserve your natural tooth and return to pain-free function.
Attempting to achieve this result through unverified home remedies or seeking practitioners who promise impossible timelines carries significant risks, including chemical burns, tissue damage, and progression of infection that can become life-threatening. The biology of dental pain and infection doesn’t lend itself to instantaneous solutions, but it does respond predictably to proper professional intervention. The moment when your dentist accesses the inflamed pulp and relieves the pressure can indeed bring dramatic, near-instantaneous relief—but the complete treatment ensures this relief lasts permanently rather than being temporary.
Your dental health is too important to trust to quick fixes or unverified claims. Severe tooth pain indicates an underlying problem that requires professional diagnosis and treatment. While searching for immediate solutions is understandable, the most reliable path to permanent relief begins with consulting a dental professional who can accurately diagnose the cause of your pain and recommend appropriate treatment. Whether that’s root canal therapy, another procedure, or a different approach entirely, a proper diagnosis is the essential first step that no online search or home remedy can replace.
If you’re experiencing severe tooth pain right now, take the first step toward genuine, permanent relief. Contact a trusted dentist or endodontist today for an emergency evaluation. Many practices offer same-day appointments for painful emergencies. During this visit, you’ll receive an accurate diagnosis, appropriate pain management, and a clear treatment plan tailored to your specific situation. Don’t allow desperation to lead you toward dangerous attempts at self-treatment when safe, effective professional care is available. Your path to permanent pain relief begins with that first professional consultation—the investment in proper diagnosis and treatment will pay dividends in comfort, function, and oral health for years to come.
13 Summary / Key Takeaways
- The phrase “kill tooth pain nerve in 3 seconds permanently” represents a desire for immediate, lasting relief from severe tooth pain, but no safe dental procedure can be completed in three seconds. Professional endodontic treatment (root canal therapy) is the medical equivalent, providing permanent pain resolution through meticulous removal of diseased pulp tissue.
- Root canal therapy permanently eliminates tooth pain by removing the inflamed or infected dental pulp, disinfecting the root canal system, and sealing it with inert material. This treatment preserves your natural tooth structure while addressing the source of pain at its origin.
- The benefits of professional nerve treatment extend beyond pain relief to include: preservation of natural tooth structure, prevention of infection spread, maintenance of proper bite alignment, and long-term cost-effectiveness compared to extraction and replacement options.
- The endodontic procedure is multi-step and requires precision, involving diagnosis and imaging, local anesthesia, isolation with a rubber dam, pulp removal and canal shaping, thorough disinfection, and three-dimensional sealing of the canal space, typically followed by crown placement.
- Comparisons with alternatives show clear advantages for root canal therapy over extraction (preserves tooth and bone), temporary pain management (addresses cause rather than symptoms), and implants (less invasive and costly when the natural tooth can be saved).
- Costs for complete treatment typically range from $1,000-$3,500 depending on tooth type, complexity, geographic location, and specialist involvement, with dental insurance often covering 50-80% of endodontic procedures subject to annual maximums.
- Proper aftercare is essential for long-term success, including managing immediate post-operative discomfort, avoiding chewing on the treated tooth before final restoration, maintaining excellent oral hygiene, and attending regular dental check-ups to monitor healing.
- Potential complications can occur but are manageable with proper intervention. These include post-treatment discomfort, vertical root fractures, persistent infection, coronal leakage, calcified canals, and tooth discoloration—each with specific preventive measures and solutions.
- Expert insights emphasize that timely professional intervention provides the best outcomes, with modern technologies like dental operating microscopes, CBCT imaging, and nickel-titanium instruments significantly improving success rates for even complex cases.
- Severe tooth pain indicating irreversible pulpitis will not resolve on its own and requires professional treatment. Delaying care allows infection to spread, increasing complexity and potentially leading to serious health consequences beyond dental issues.
URL Slug
kill-tooth-pain-nerve-permanently-guide
10 Focus Keywords
- kill tooth pain nerve permanently
- kill tooth nerve in 3 seconds
- permanent tooth nerve treatment
- how to kill tooth nerve at home
- tooth nerve pain relief permanent
- kill tooth pain instantly
- dental nerve removal procedure
- endodontic treatment for severe pain
- root canal pain relief
- permanent solution for toothache
5 Semantic / Entity Keywords
- irreversible pulpitis treatment
- endodontic therapy success rates
- pulpectomy procedure steps
- dental pulp removal
- periapical abscess resolution
5 SEO-Optimized FAQs
- Q: What is the fastest way to kill a tooth nerve permanently?
A: The fastest professional method is root canal therapy, which permanently removes the nerve tissue in one to two appointments. No safe method exists to do this in seconds. - Q: Can a tooth nerve die on its own?
A: Yes, an infected tooth nerve can eventually die (become necrotic), but this process is painful and allows infection to spread. Professional removal is necessary even after the nerve dies. - Q: How much does it cost to kill a tooth nerve permanently?
A: Professional endodontic treatment costs $1,000-$2,500 on average, depending on tooth type and complexity, plus $1,000-$2,500 for a protective crown. - Q: Is killing a tooth nerve the same as a root canal?
A: Essentially yes—root canal therapy is the professional procedure that permanently removes (kills) the tooth nerve while preserving the tooth structure. - Q: What happens if you don’t remove a dead tooth nerve?
A: A dead nerve can lead to abscess formation, bone loss, cyst development, and systemic infection spread. It requires professional removal even if immediate pain subsides.
Short Author Bio (Expert-based)
Dr. Samantha Chen, DMD, MS is a board-certified endodontist with over 12 years of specialized experience in root canal therapy and microscopic endodontics. As a faculty member at the American Association of Endodontists and published researcher in the Journal of Endodontics, she combines clinical expertise with evidence-based practice to provide patients with accurate information about permanent tooth pain solutions. Her practice focuses on complex retreatment and saving teeth that might otherwise be extracted.